Nerve blocks have gained widespread acceptance as tools for maximizing perioperative and chronic pain control while minimizing opioid consumption. Ultrasound-guided interscalene blocks present numerous benefits and opportunities for optimising care in patients undergoing shoulder, upper arm, or elbow surgery. Read on to gain an overview of nerve blocks and learn how ultrasound guidance can greatly increase the benefits of interscalene blocks and other perioperative procedures.
Nerve blocks: A fundamental pillar in opioid-free anaesthesia protocols
Setting the stage– The worst drug crisis in American history
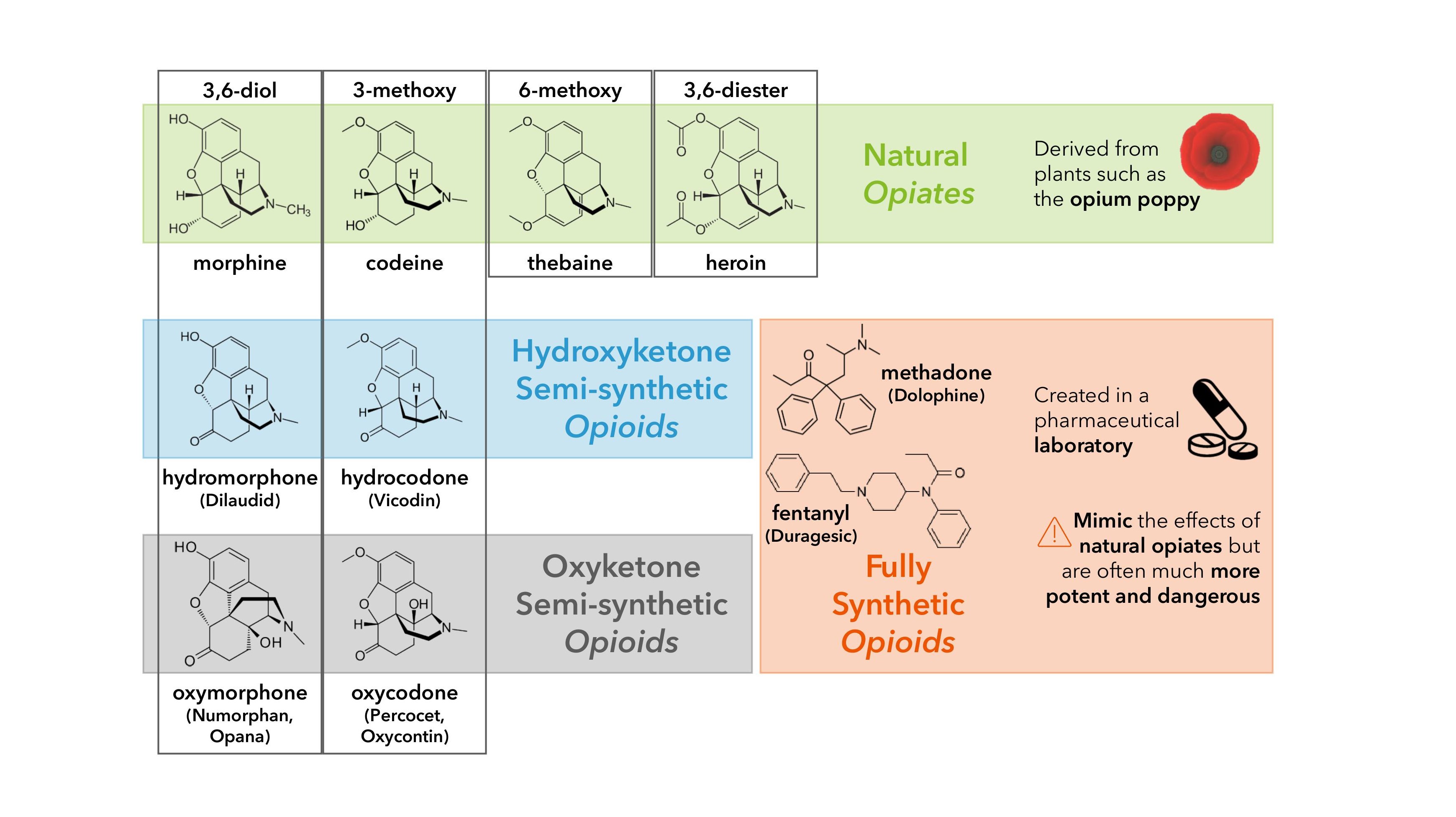
Natural opiates have been an integral part of pain treatment strategies for millennia.1 Although originally introduced in surgical anaesthesiology as an adjunct, synergistic agent of volatile anaesthetics in the nineteenth century,2, 3 the use of synthetic opioids at high doses during surgery was not fully adopted until the 1960s.4 The late 1990s brought about a sharp increase in opioid prescriptions for perioperative pain control, followed by their widespread acceptance and use for the treatment of chronic pain.5
This flood of prescribed opioids, which continues to increase substantially every year,6 has led to a surge of addiction7 and a parallel, steady rise in overdose fatalities.8 Despite long-standing controversy regarding risk and long-term effectiveness,9 studies have definitely shown that opioids medications can lead to dependency within a matter of days,10 and ~25% of patients who receive long-term opioid therapy become addicted.11 12 13 Since 1999, more than half a million people have died from a drug overdose involving prescription and illicit opioids.8 With opioid-related overdose deaths reaching historic highs,14 the nationwide opioid addiction epidemic was declared a national emergency in 2017.15
For many patients with opioid use disorder, the perioperative period represents the initial exposure and an important source of unused prescription opioids.16 Modern approaches therefore seek to reduce opioid use in favour of multimodal pain management protocols.17 Nerve blocks have emerged as an attractive option in opioid-sparing analgesia strategies. As technological advancements improve on their accuracy, efficacy, and safety, the use of nerve blocks continues to expand, offering superior pain control in various surgical and pain management procedures.18 19
What is a nerve block?
Nerve blocks, or neural blockades, deliberately interrupt the transmission of signals traveling along a specific nerve or group of nerves to temporarily reduce or eliminate pain in specific parts of the body during and after surgery (e.g., procedural anaesthesia and perioperative analgesia), as well as for the treatment of chronic, long-term pain.20 These procedures offer immediate pain relief that can be temporary (hours) or long-lasting (months), depending on the medication and the technique used.
What types of nerve blocks are there?
Nerve blocks can consist of sympathetic blockades,21 where anaesthetic agents are injected onto or near a nerve to block pain; or neuroablation,22 involving the targeted destruction of a nerve or nerve plexus via chemical, thermal, or surgical methods.
Depending on their purpose, nerve blocks are grouped into 3 main categories:23
- Therapeutic: used to treat chronic pain and various conditions or injuries involving damaged, inflamed, or irritated nerves.
- Diagnostic: used to identify the source of pain.
- Prognostic: used to determine if a permanent solution like surgery would be a successful pain management strategy.
Interscalene blocks: Challenges and opportunities
Peripheral nerve blocks are now a common component of multimodal analgesia for upper24 and lower25 extremity surgical procedures. Interscalene blocks26 target the brachial plexus, a network of nerves that innervate the shoulder and upper limb, to provide dense surgical anaesthesia and/or perioperative analgesia for distal clavicle, shoulder, and proximal humerus procedures.
Ultrasound guidance of interscalene blocks lead to improved patient outcomes
Ultrasound imageing is increasingly used to guide peripheral nerve blocks, and presents numerous advantages compared to other traditional approaches. Ultrasound is a safe, portable, and easily accessible imageing modality that carries no risk of ionising radiation. It enables real-time visualisation of neural and surrounding structures, needle advancement, and local anaesthetic spread to maximize success, reduce performance time, and minimize complications27
Interscalene blocks are commonly performed under sterile conditions in the preoperative suite or postanaesthesia care unit with the patient mildly sedated. Ultrasound guidance is used to correctly identify the brachial plexus roots within the interscalene groove, helping guide needle placement and avoid intravascular spaces. A nerve stimulator may also be used as an adjunct to confirm placement, causing muscle contractions in the appropriate muscle when the corresponding nerve is stimulated. Once the needle position is confirmed, a volume of local anaesthetic is administered, and the needle is removed. The patient can expect pain relief and limb heaviness for the duration of local anaesthetic action, typically 4–24 hours.
Benefits of ultrasound guidance in interscalene blocks:
- Faster onset time and longer duration, produces surgical anaesthesia more reliably for the same volume of local anaesthesia compared to nerve-stimulation28
- Can decrease incidence of hemidiaphragmetic paresis29
- Lower volumes of local anaesthetic are needed for an effective block30
- May reduce the risk of nerve injury31
- Inhibition of the nociceptive impulse may decrease the occurrence of muscle spasm following mobilisation postoperatively, which may contribute to improved functional recovery32
What are its limitations and risks?
Regardless of the technique or block location, nerve block risks include vascular puncture and bleeding, nerve damage, and local anaesthetic systemic toxicity.
Interscalene blocks are generally safe. Common complications include:
- Bleeding or infection at the site
- Recurrent larungeal nerve blockage
- Allergic reaction
- Horner syndrome - a rare condition that causes disruption of nerve pathways from the brain to face and eyes
- Hematoma
Other rare but severe complications include:
- Permanent brain damage
- Bradycardia (slow heartbeat)
- Pneumothorax (collapsed lung)
- Severe hypotension (low blood pressure)
- Cartoid artery puncture
The ability to track the needle tip, assess local anaesthetic spread, and maintain cautious approach to nerve roots and vascular structures that is afforded by ultrasound guidance are fundamental to reducing the risk of complications outlined such as nerve injury or local anaesthetic toxicity outlined above.
Additional Resources
Learn more about ultrasound guidance and how it can greatly increase the benefits of interscalene blocks and other perioperative procedures at the Sonosite Institute for Point-of-Care Ultrasound, an in-depth educational resource provided exclusively to Sonosite customers where you can enhance your skill set, monitor your progress through each course, and earn certificates of completion.
1. Rosenblum A, Marsch LA, Joseph H, Portenoy RK. 2008. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol 16(5):405-16, PMID: 18837637, https://doi.org/10.1037/a0013628.
2. Torri G. 2010. Inhalation anaesthetics: a review. Minerva Anestesiol 76(3):215-28, PMID: 20203550.
3. James A, Williams J. 2020. Basic Opioid Pharmacology - An Update. Br J Pain 14(2):115-121, PMID: 32537150, https://doi.org/10.1177/2049463720911986.
4. Forget P. Opioid-free anaesthesia. Why and how? A contextual analysis. 2019. Anaesth Crit Care Pain Med 38(2):169-172, PMID: 29775728, https://doi.org/10.1016/j.accpm.2018.05.002.
5. Rosenblum A, Marsch LA, Joseph H, Portenoy RK. 2008. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol 16(5):405-16, PMID: 18837637, https://doi.org/10.1037/a0013628.
6. Guy GP Jr, Zhang K, Bohm MK, Losby J, Lewis B, et al. 2017. Vital Signs: Changes in Opioid Prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep 66(26):697-704, PMID: 28683056, https://doi.org/10.15585/mmwr.mm6626a4.
7. Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. 2003. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug Alcohol Depend 69(3):215-32, PMID: 12633908, https://doi.org/10.1016/s0376-8716(03)00003-6.
8. Centres for Disease Control and Prevention (CDC). 2021. Wide-ranging online data for epidemiologic research (WONDER). [Website] Atlanta, GA: CDC, National Centre for Health Statistics. Available at http://wonder.cdc.gov [accessed 2022 Dec 27].
9. Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, et al. 2008. Opioid complications and side effects. Pain Physician 11(2 Suppl):S105-20, PMID: 18443635.
10. Shah A, Hayes CJ, Martin BC. 2017. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use — United States, 2006–2015. MMWR Morb Mortal Wkly Rep 66(10):265–269, PMID: 28301454, https://doi.org/10.15585/mmwr.mm6610a.
11. Banta-Green CJ, Merrill JO, Doyle SR, Boudreau DM, Calsyn DA. 2009. Opioid use behaviours, mental health and pain—development of a typology of chronic pain patients. Drug Alcohol Depend 104:34–42, PMID: 19473786, https://doi.org/10.1016/j.drugalcdep.2009.03.021.
12. Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, et al. 2010. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction 105(10):1776-82, PMID: 20712819, https://doi.org/10.1111/j.1360-0443.2010.03052.x.
13. Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. 2007. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain 8(7):573–82, PMID: 17499555, https://doi.org/10.1016/j.jpain.2007.02.432.
14. Hedegaard H, Miniño AM, Spencer MR, Warner M. 2021. Drug Overdose Deaths in the United States, 1999–2020 [PDF]. National Centre for Health Statistics (NCHS). Available from: https://www.cdc.gov/nchs/data/databriefs/db428.pdf [accessed 2022 Dec 15].
15. Gostin LO, Hodge JG Jr, Noe SA. 2017. Reframing the Opioid Epidemic as a National Emergency. JAMA 318(16):1539-1540, PMID: 28832871, https://doi.org/10.1001/jama.2017.13358.
16. Soffin EM, Lee BH, Kumar KK, Wu CL. 2018. The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth 122(6):e198-e208, PMID: 30915988, https://doi.org/10.1016/j.bja.2018.11.019.
17. Ljungqvist O, Francis NK, Urman RD (Eds). Enhanced recovery after surgery: a complete guide to optimising outcomes. 1st ed. Switzerland: Springer; 2020.
18. Joshi G, Gandhi K, Shah N, Gadsden J, Corman SL. 2016. Peripheral nerve blocks in the management of postoperative pain: challenges and opportunities. J Clin Anesth 35:524-529, PMID: 27871587, https://doi.org/10.1016/j.jclinane.2016.08.041.
19. McLott J, Stahel PF. 2022. Opioid-free anaesthesia: the next frontier in surgical patient safety. Patient Saf Surg 16(1):38, PMID: 36461121, https://doi.org/10.1186/s13037-022-00346-5.
20. Wiederhold BD, Garmon EH, Peterson E, et al. 2022. Nerve Block Anaesthesia. In: StatPearls [Website]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431109/ [updated 2022 Sep 26].
21. Doroshenko M, Turkot O, Horn DB. 2022. Sympathetic Nerve Block. In: StatPearls [Website]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557637/ [updated 2022 Nov 17].
22. Gupta A, Earls B. Neuroablation Techniques for Pain Management. In: Banik RK (Ed), Anaesthesiology In-Training Exam Review. Springer, Cham; 2022. https://doi.org/10.1007/978-3-030-87266-3_63
23. Levy BA. 1977. Diagnostic, prognostic, and therapeutic nerve blocks. Arch Surg 112(7):870-9, PMID: 880030, https://doi.org/10.1001/archsurg.1977.01370070084014.
24. Srikumaran U, Stein BE, Tan EW, Freehill MT, Wilckens JH. 2013. Upper-extremity peripheral nerve blocks in the perioperative pain management of orthopaedic patients: AAOS exhibit selection. J Bone Joint Surg Am 95(24):e197(1-13), PMID: 24352782, https://doi.org/10.2106/JBJS.L.01745.
25. Stein BE, Srikumaran U, Tan EW, Freehill MT, Wilckens JH. 2012. Lower-extremity peripheral nerve blocks in the perioperative pain management of orthopaedic patients: AAOS exhibit selection. J Bone Joint Surg Am 94(22):e167, PMID: 23172334, https://doi.org/10.2106/JBJS.K.01706.
26. Zisquit J, Nedeff N. 2022. Interscalene Block. In: StatPearls [Website]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519491/ [updated 2022 Sep 19].
27. Sites BD, Antonakakis JG. 2009. Ultrasound guidance in regional anaesthesia: state of the art review through challenging clinical scenarios. Local Reg Anesth 2:1-14, PMID: 22915860, https://doi.org/10.2147/lra.s3444.
28. Kapral S, Greher M, Huber G, Willschke H, Kettner S, et al. 2008. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med 33(3):253-8, PMID: 18433677, https://doi.org/10.1016/j.rapm.2007.10.011.
29. Liu SS, Zayas VM, Gordon MA, Beathe JC, Maalouf DB, et al. 2009. A prospective, randomised, controlled trial comparing ultrasound versus nerve stimulator guidance for interscalene block for ambulatory shoulder surgery for postoperative neurological symptoms. Anesth Analg 109(1):265-71, PMID: 19535720, https://doi.org/10.1213/ane.0b013e3181a3272c.
30. McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, et al. 2011. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth 106(1):124-30, PMID: 21059701, https://doi.org/10.1093/bja/aeq306.
31. Szerb JJ, Greenberg JL, Kwofie MK, Baldridge WH, Sandeski RE, et al. 2015. Histological confirmation of needle tip position during ultrasound-guided interscalene block: a randomised comparison between the intraplexus and the periplexus approach. Can J Anaesth 62(12):1295-302, PMID: 26335906, https://doi.org/10.1007/s12630-015-0468-y.
32. Héroux J, Belley-Côté E, Echavé P, Loignon MJ, Bessette PO, et al. 2019. Functional recovery with peripheral nerve block versus general anaesthesia for upper limb surgery: a systematic review protocol. Syst Rev 8(1):273, PMID: 31711533, https://doi.org/10.1186/s13643-019-1204-4.

