Anesthesiologist Dr. Frances Chow works to bring ultrasound-guided nerve blocks to British Columbia Cancer Agency, Vancouver, BC, Canada. British Columbia Cancer Agency has among the best cancer outcomes in the world, including highest of the G7 countries for childhood leukemia, and second highest survival rates across 67 countries for prostate and breast cancer.[1]
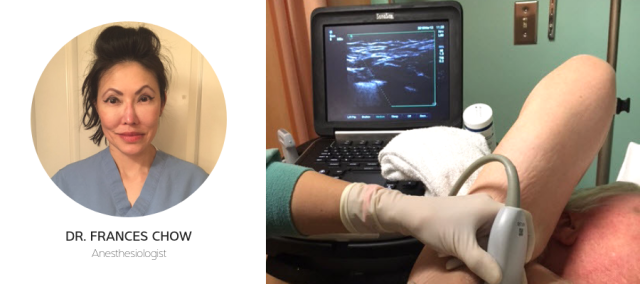
BC Cancer covers the entire spectrum of cancer care, from prevention and screening to diagnosis, treatment, and rehabilitation. They operate six regional cancer centers and are dedicated to finding the causes of cancer, and creating a better quality of life for their patients.This search for improved patient care and outcome is what led Dr. Frances Chow to seek new methods for pain management and surgical anesthesia, and her search led her to seek training in ultrasound-guided nerve blocks with FUJIFILM Sonosite.
After training, Dr. Chow approached the Surgical Oncology team at BC Cancer with a plan to use pectoral nerve blocks (PECS blocks) on patients who could not tolerate general anesthesia due to their medical comorbidities and potentially higher risk of complications. Dr. Chow performed a clinical study to assess the benefits of using PECS blocks over general anesthesia, reduce the use of opioids for pain management, and decrease morbidity related to general anesthesia. Dr. Chow believed that these blocks could enhance patient experience, decrease opioid use, and provide a solution for high-risk patients.
After using PECS blocks on over 200 cases, the surgical oncology team began requesting blocks for patients who do not have medical comorbidities, but for whom optimal pain control, or avoidance of general anesthesia side effects, were sought.
Dr. Chow is currently expanding her use of ultrasound-guided blocks in other surgical regions. She has started performing blocks for surgeries such as lymph node biopsies, tumor excisions in limbs, trunk and pelvic regions, and for brachytherapy of genital cancers.
Dr. Chow established the Regional Anesthesia Block Program at the Vancouver BCCA Surgical Oncology Suite in September 2016.
Ultrasound-guided regional blocks are clinically useful for pain management in surgical patients. They decrease recovery room workload since our patients needed little-to-no intra-op or post-op narcotics, for pain management. This leads to less sedation, and less nausea and vomiting.
I recently had an obese 80-year old patient who was scheduled for a diagnostic left axillary mass removal. She had sleep apnea, MI, A.fib, IDDM, higher BMI – 37, hypertension, and lymphoma. General anesthesia at a daycare surgical facility such as BCCA was not a safe option. Surgical left axillary mass excision done under PEC regional block. Excellent surgical conditions provided, patient did not have any pain intra-op or post-op, uneventful surgical and anesthesia outcome, same-day discharge. Post-op follow-up – no pain for 23 hours post-op and no analgesics needed post discharge home. We could not have done this block without the Sonosite ultrasound.
I had another patient who was obese, BMI 45, OSA, HT, and restrictive lung function with breast CA requiring fine wire-guided lumpectomies. I performed a PEC block instead of GA, avoiding the need for post-op ventilatory assistance and an overnight stay.
During my clinical study, I found that by using Sonosite ultrasound systems for regional blocks, I could achieve:
- Surgical anesthesia for medically complex patients requiring surgical diagnosis or treatment of cancer
- Good to Excellent perioperative pain management, often patients need no analgesics postop
- Fewer opioids (or no opioids) prescribed to patients for post-op pain
- Avoidance of over-sedation and hypoventilation in patients post-op
- Decreased times to full alertness post-surgery and discharge criteria with faster returns to mobility
- Improved respiratory function and no atelectasis during recovery
- Same-day discharge for patients, no cases of unanticipated overnight admission, unless scheduled to stay overnight, for example mastectomy
I can perform an ultrasound-guided PECS block in 6-10 minutes the majority of the time, from probe-on-skin to probe-off.
The time savings comes from no induction time in the OR, and no wake up time. The nurses in pre-op can prep the patient, I arrive in the pre-op regional block area and do the block, patient’s anesthesia established, and the patient is ready for surgery.
My patients have good experiences with the pain control post-op. Vancouver BCCA has a large patient referral base from all over Canada. Our out-of-town patients find that they can even travel home by plane, ferry, or car, within hours of surgery without pain, nausea, or vomiting.
Surgeons and nursing staff are pleased with increased efficiency and time savings. I am very appreciative of the surgeons and nursing staff for supporting ultrasound-guided regional blocks for patient care.
I cannot imagine my anesthesia practice without ultrasound-guided regional blocks; they are my anesthetic technique of choice for medically complicated patients requiring surgical daycare procedures.
[1] http://www.phsa.ca/our-services-site/Documents/Fact%20Sheet%20BCCA.pdf
