S Series: Brachial Plexus Supraclavicular Level 1
S Series: Brachial Plexus Supraclavicular Level 1

/sites/default/files/201410_Image_S-System_Brachial_Plexus_Supraclavicular_Level_1.jpg
S Series: Brachial Plexus Supraclavicular nerve block Level 1.
Clinical Specialties
Media Library Type
Media Library Tag
Body
S Series: Brachial Plexus Supraclavicular nerve block Level 1.
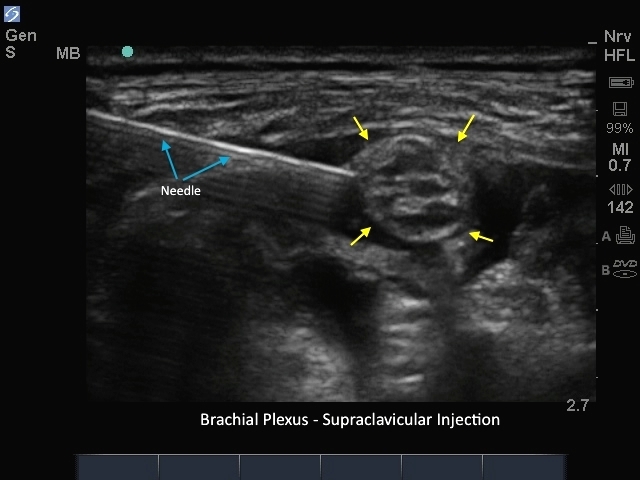
M-Turbo: Brachial Plexus Supraclavicular Injection
M-Turbo: Brachial Plexus Supraclavicular Injection
/sites/default/files/201410_Image_M-Turbo_Brachial_Plexus_Supraclavicular_Injection.jpg
M-Turbo: Brachial Plexus Supraclavicular nerve block.
Clinical Specialties
Media Library Type
Media Library Tag
Body
M-Turbo: Brachial Plexus Supraclavicular nerve block.
M-Turbo: Axillary Nerve Post Injection
M-Turbo: Axillary Nerve Post Injection

/sites/default/files/201410_Image_M_Turbo_Axillary_Nerve_Post_Injection2.jpg
M-Turbo: Axillary Nerve Post Injection.
Clinical Specialties
Media Library Type
Media Library Tag

