Com uma pressão constante sobre os prestadores de cuidados de saúde para melhorar a qualidade e a eficiência dos tratamentos ao mesmo tempo em que reduz os custos, a padronização da gestão do paciente é um passo lógico em direção à maior otimização dos serviços. A área da anestesia é uma que está começando a adotar essa abordagem, combinando bloqueios regionais de nervos com orientação de ultrassom para melhorar a qualidade e a eficácia do atendimento ao paciente, enquanto reduz as permanências no hospital.
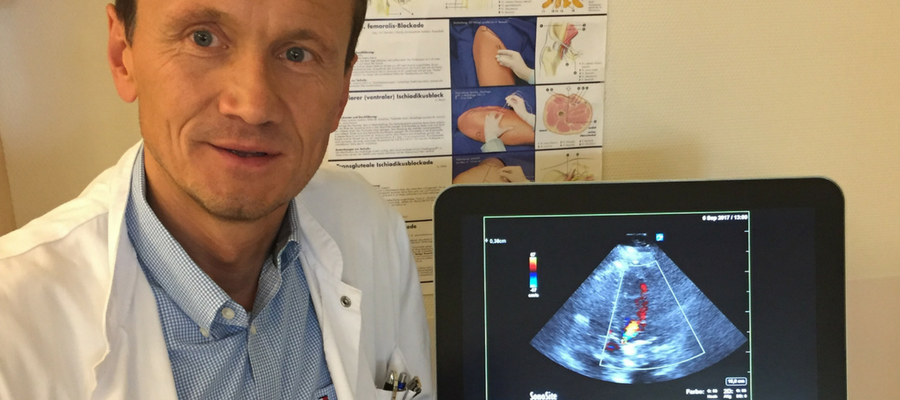
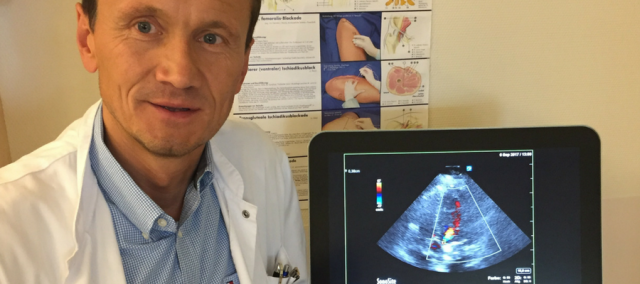
O Dr. Martin Zoremba (PhD), escrivão chefe do departamento de anestesia no Kreisklinikum Siegen, descreve a transformação do seu departamento e os benefícios que uma abordagem padronizada oferece.
Cirurgia ambulatorial é um bom exemplo de como práticas de cuidados de saúde estão mudando para proporcionar redução de custos, melhorando a satisfação e o atendimento ao paciente. Amplamente considerada como uma maneira mais eficiente de realizar muitas operações menores, essa abordagem é baseada no uso de bloqueios regionais dos nervos como alternativa à anestesia geral. Isso ajuda a encurtar o tempo das recuperações – muitas vezes possibilitando que os pacientes voltem para casa no mesmo dia – e evita as potenciais complicações associadas à anestesia geral, além de proporcionar melhor controle da dor pós-operatória.
Bloqueios regionais também podem melhorar a segurança e simplificar a gestão de pacientes de alto risco, tornando a técnica especialmente útil para intervenções urgentes em pacientes com trauma.
Apesar dessas vantagens, muitos hospitais em toda a Europa ainda não adotaram plenamente a anestesia regional. Há uma variedade de razões para isso, incluindo a falta de financiamento para os sistemas de ultrassom a beira do leito (POC) necessários para realizar bloqueios regionais com rapidez e eficácia, pouca compreensão sobre os benefícios para o fluxo de trabalho e uma resistência à mudança das práticas convencionais, de dentro e fora do departamento de anestesia.
O Dr. Martin Zoremba é o principal entusiasta dessa abordagem, recebendo um PhD em hemodinâmica perioperatória e anestesia regional usando ultrassom no hospital universitário de Giessen e Marburg. Desde que se mudou para Kreisklinikum Siegen em 2015, ele reformulou completamente como o departamento funciona, introduzindo o ultrassom POC para anestesia regional e padronizando as práticas para muitos dos protocolos dos departamentos.
“When I arrived in the department,” says Dr. Zoremba, “there was very little regional anesthesia being performed, and no use of POC ultrasound. Based on my experiences in Marburg, I knew the benefits that this approach could bring to both patient care and the department’s workflow, and immediately began training the anesthesia team here to perform ultrasound-guided regional blocks. We also created SOPs for many of our activities within the department, including how and when ultrasound should be used.”
Within a year, the department had switched to regional anesthesia for a large proportion of procedures. This dramatic change in how the department operates initially met with some resistance, but the benefits quickly became clear.
“SOPs make it very clear for everyone what the correct protocol is, simplify decision making, and help to improve the flow of patients, explained Dr. Zoremba. “This ensures a consistently high level of care and allows the department to run efficiently while still meeting the individual needs of each patient. Successfully converting to this type of approach requires both staff and management buy-in and, just as importantly, clear goals from the outset.
“For example, within our department, the economic argument for switching to ultrasound-guided regional anesthesia and pain control was very clear. Every day a patient spends in hospital costs approximately €500 so, even if we only shorten each patient’s stay by one day, that saves over €1 million for the 3-4,000 orthopedic and trauma patients we treat each year. Equally importantly, the changes we have implemented have led to improved patient satisfaction and a much smoother flow of patients, so staff can clearly see the advantages.”
Dr. Zoremba attributes this rapid turnaround to an intensive training program and the ease of use of the department’s POC ultrasound systems like the Sonosite X-Porte.
“We use a ‘landmark’ based anatomical approach, making it easy for even novice ultrasound users to quickly learn to locate the nerves and guide the needle to the injection site. We combine this with an in-plane technique using a Sonosite X-Porte’s excellent linear transducer, as this offers very good needle visualization, even for inexperienced users.
“We can perform over 99% of all blocks this way – even very deep blocks and sciatic blocks – which is both fast and efficient, and avoids the use of nerve stimulators, improving patient comfort. Each anesthetist in the department has been trained in this way, and newly qualified junior doctors coming through the department undertake a 3-week POC ultrasound boot camp with 1-on-1 training in ultrasound-guided blocks with a senior physician.
“Our X-Porte systems are ideal teaching tools, and represent one of the most complete devices on the market for anesthesia. The touchscreen interface is also very good, making it easy to optimize images, and being very easy to clean. Just as importantly, the versatility of the ultrasound system allows us to perform other types of ultrasound scan – particularly transthoracic echocardiography (TEE) for the hemodynamic management of trauma patients.
“Perioperative TEE evaluation using the X-Porte can be easily implemented, allowing optimized, patient-specific risk management and treatment. This avoids overloading the patient with anesthetic, shortening recovery times and hospital stays, which also helps to reduce pressure on post-operative intensive care resources. It’s good for both the patient and the hospital.
“Changing even small elements of workflows can benefit a whole department, and many anesthesia department leaders will likely have had similar ideas. Unfortunately, resistance to changing long-established individual practices can be a significant challenge; many good ideas have never been implemented due to a lack of resources or support, either internal or external.”
To help address this, Dr. Zoremba’s team has recently developed a new anesthesia workshop – “to our knowledge, the only one of its kind in Europe,” says Dr. Zoremba – which focuses on implementing POC ultrasound skills.
“Combining theoretical and hands-on ultrasound training with sessions on change management,” says Dr. Zoremba, “will hopefully enable more anesthesia departments to benefit from the use of regional anesthesia.”
Learn More About the Sonosite X-Porte
Anesthesiologists who utilize ultrasound guidance for needle placement see a decrease in vascular puncture and an increase in the effectiveness of pain management medication, Intuitive Touchscreen Interface, and the Sonosite X-Porte's intuitive touchscreen interface allows anesthesiologists to easily customize the user interface to suit their needs.